Some words of introduction on this new series from the digital health sector @ Arkin Holdings
A 1000-ish monthly posts on trends, opportunities and challenges in digital health as we at Arkin see them. Our goal here is to share our take on the digital health realm and highlight what makes us tick and what doesn’t.
We aim both to provide some added value and to find new partners who share similar points of view - entrepreneurs, fellow investors, industry leaders, …
A bit cynical and a bit provocative but hopefully constructive :)
Want to receive updates on news posts?
This post will deal with the notorious field of telehealth and will hopefully tease out some truth from A LOT of noise and hype. Let’s get started.
What is telehealth and why it looks like the coolest (new?) kid in town?
Telehealth, or the administration of health services remotely (Namely, patient-physicians “virtual encounters”), has actually been around about three decades (for example, check this JAMA review from 1995) yet in the beginning of 2020, it was still very underutilized – estimated to be around roughly 1% of medical encounters.
Then along came COVID, and the utilization of telehealth finally reached a critical mass. COVID created strong tailwinds but at least some of the positive factors have already been building up even before thus creating a perfect storm (well, at least for a while). Hereby are some of the key factors -
Favorable regulatory environment, such as waiving limitations on geography and originating site restrictions. Physicians can now provide telehealth for patients outside the state of their practice (as MD licenses are administered per specific state) and can provide telehealth to their patients directly (and not via a telehealth platform).
Supporting reimbursement – adding >135 reimbursable telehealth services, broader mandate to reimburse for telehealth from any certified provider, expending “hospital without walls” initiatives for acute hospitalizations at home and more.
Reduction of the in-person alternative, due to the combination of the prohibiting in-person visits for a large period of time together with social distancing and patients fear of being exposed to COVID-19 when entering a clinic or a hospital.
Improved data interoperability (well, to some extent) – The 21st Century Cures Act has perhaps paved the way for long awaited changes of data exchange between different stakeholders. But even before these changes start to kick in (early next year as the first step for provider–patient data sharing, but some others only in years to come), there is already small, yet meaningful data integration and migration plays that makes telehealth much more efficient. To name just one, connecting between the telehealth platform and the provider’s EHR is crucial to create encounters that are actually built within the workflow with the prerequisite of screen-to-screen copy paste.
Technology maturation – enhanced access to video streaming (by smartphones or desktop), internet bandwidth, etc.
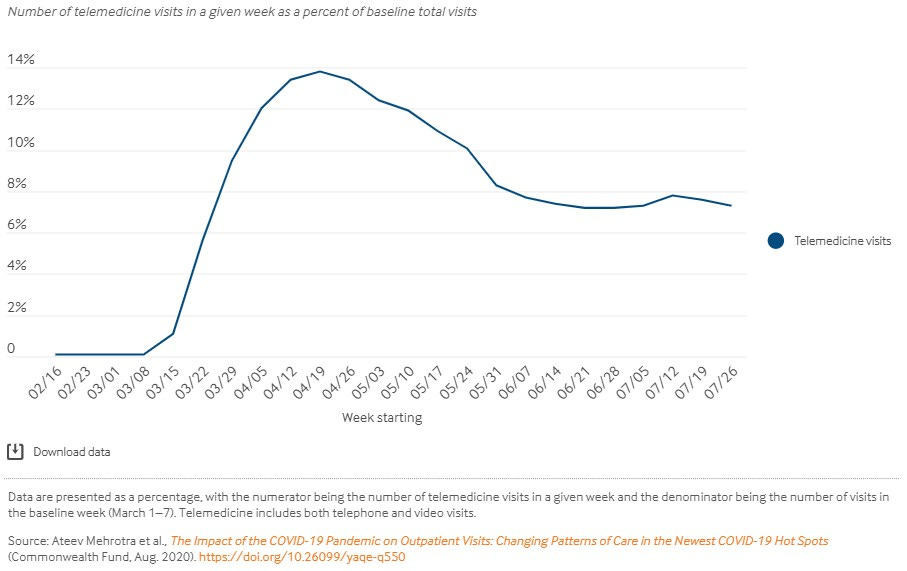
Consequently, Telehealth usage exploded in the initial months of the first wave of COVID-19, and even though usage has decreased to ~10% - 15% recently, it is still ~x10 compared to early 2020.
But Why in fact, the situation is not that positive?
For starters, there is concern that much of the aforementioned changes will not endure. One example is the reimbursement rate per virtual encounter vs. in-person. Currently they are equal, even though in-person costs for providers are much higher. Consequently, several commercial health plans have already notified they will no longer fully reimburse virtual visits under certain circumstances by early 2021 and CMS is expected to follow. Even on the regulatory side, there is still no clarity about how post COVID-19 regulation will look like (and much is dependent on the bipartisan bill Protecting Access to Post-COVID-19 Telehealth Act that was introduced back in July).
But even if we put these questions aside, there are still inherent limitations in the current form of telehealth that hinder many types of health encounters to be truly equivalent to in-person visits.
Lack of holistic physical examination. From the very early days of medical school, we were taught first to examine (the patient and to an equal degree her/his environment), ask and then touch. In my med school (Ben Gurion Uni.) the patient-first approach was strictly enforced - skipping any steps and going to labs or imaging was considered a grave failure. However, that’s exactly the case with telehealth. No physical exam and no chance to the see the patient’s surroundings (even the clothes they wear). Now, one may claim that some types of encounters do not necessitate a physical exam (like mental health or dermatology) but just think about all these mental conditions that are actually caused by “organic” pathophysiology (vitamin deficiencies, liver dysfunction and many more) that could easily be assessed by a short “physical”. On top of that, when physicians (who in most cases in telehealth are not the regular physician of the patient) can’t do their work to it’s fullest, protective measures come into play and you get unnecessary lab work and E.D. admissions that could be avoided. For sure there is a valid argument around augmenting / decision support devices such as iRhytm’s Zio or Tyto that mitigate at least some of the problem. Perhaps I’ll deep dive there in a future post.
Lack of sufficient information – following the previous point, a proper medical encounter starts from knowing the medical history. Nothing can compare between a chest pain in patient who underwent MI a year ago to another with a history of gastric reflux. And with all the talks around interoperability, we are still SO far from there… In most cases just overcoming the IT barrier of legacy EHR systems is simply impossible, let alone integration of different monitoring devices. I truly believe we will get better in this aspect, but it will take more time and resources than expected.
Lack of trust. Good medicine is based on trust, and perhaps even the entire healthcare industry. I will address the importance of trust in future posts but IMO it is the very foundation of the system. Only IF the patient trusts the physician there is a true opportunity to capture all the relevant information, make the right diagnosis and treatment plan. As countless studies have proven, physical contact is key to create trust.
Lack of the “extra mile”. In some cases, healthcare encounters are not just about solving a discrete medical need. Just look at the difference in two patients presented with the same chief compliant where one is 80 years old and the other is 55. Good chance the 80 years old will look for companionship and perhaps a friendly ear to his other hardships, even if unconsciously. Loneliness is a HUGE problem, especially in Medicare population and reducing it via “non-medical” chat has also “medical” benefits… Patients are less inclined to do that outside the physical environment. Again, the trust issue.
Lack of support for several key target populations. One of the great promises of telehealth is reducing healthcare related disparities by allowing high-end care for rural and poor populations, who lack access to top tier medical facilities. However, when you deep dive into utilization data, you see that people comfortable with tech and with proper access to video streaming (by large, those from high socio-economic backgrounds and not your average Medicare or Medicaid beneficiary) are much more prone to using telehealth services. I led a big study at Clalit Health Services (largest payer-provider system in Israel, providing care for >50% of the Israeli population) around its pediatric telehealth service (>500,000 virtual encounters) and we got similar results. The end game here is over utilization of health service for those who already have access (hence EXTRA cost for payers), and under utilization for those who don’t (and again, extra cost for payers due to deterioration in their health status and thus increased future expenditures). Telehealth is supposed to the target the most expensive “users” (elderly, multimorbid) and allegedly reduce costs in that manner. Nevertheless, currently it seems the very opposite is achieved.
Lack of tech margins – apparently telehealth sounds like very lucrative, high margin business. Yet “legacy” virtual care companies such as Teladoc and AmWell are consistent bleeders and despite the volume surge generated by COVID-19, their margins remained pretty much unchanged, y’-y’ and q’-q’ (GM of ~60% and ~45%, respectively). Both would still generate negative EBITDA of ~$100M in 2020. There are number of reasons for this situation that could populate another post but, in a nutshell, it seems that there is a lot of service within this tech offering.
Taking all that in mind, should telehealth companies trade at x20-30 / LTM revenues?
Telehealth 1.0 vs 2.0
Let’s try to wrap it up and have some conclusions.
We have a clear need for accessible care due to the unmatched influx of demand (chronic diseases, elderly population, consumerism of health,… ) and providers are working tooth and nail to maintain their revenues and margins (shall not say avoid bankruptcy), yet simultaneously much of the promise of telehealth hasn’t been materialized (and hopefully I’ve at least partially convinced you why). Some would say this is a dire situation, but it can also be seen as an opportunity…
IMO it does not seem like the answer would come from current market leaders. i.e., not “Telehealth 1.0” companies (TDOC, AMWL, DocOnDem, MDLive…) nor health systems trying to create virtual extensions. Given that some of the challenges listed above are here to stay in the foreseeable future, I would argue that the best model is hybrid. Virtual care (still) has too many shortcomings that are addressable via in-person and vice-versa. Therefore, it seems that converging in-person and virtual visits into a single offering managed by a single entity and thus tailoring the right settings to a specific condition in a cost-effective manner is the proper path. I would also argue that to do so in a real unbiased manner, the supplier should have a clear stake in both realms. In other words, current health systems have too many physical resources they have to justify that would hinder their ability to efficiently funnel visits to the right location. On the flip side, legacy telehealth suppliers are too invested in the opposite virtual setting. You need a real front door solution that controls the funnel from end-to-end. If it seems like I’m alluding to the liking of One Medical or Oak Street you are not mistaken. But I would place my bet elsewhere. As my runner-up I would go for a physical retail giant acquiring a telehealth entity. These guys have the real-estate but can build and craft the right kind of healthcare related physical assets. Just as an example look at the collaboration between Walmart and DocOnDem. CVS-Cigna have even a better chance due to their health plan side. But all will eventually lose to Amazon.
If we examine the requirements for an end-to-end funnel from different angles, namely establishing a true hybrid solution that encompasses physical and virtual, clinics and at home care, it seems like the Seattle Behemoth have (or can easily have) all the pieces of the puzzle. In fact, it really resembles other plays they already successfully executed.
Capability to reach the customers at their home in the most effective manner – check
Unmasking (or creating) the customer’s real needs - check
Relevant products for homecare / primary care clinics (Alexa, Halo, Amazon Pharmacy) – check
Technology infrastructure (AWS, Amazon Health Lake) - check
Physical assets, AKA “last mile clinics” – in the making, currently via partnership (Crossover health), but think about the Wholefoods play just in healthcare and you understand where they can easily go…
Innovative culture – check
Working MVP (Amazon care) – check
My point here is not to praise Amazon but to try to highlight some unmet needs in realm of telehealth, at least by our perspective. Each hurdle can be a fruitful opportunity. We are keen to partner with teams that can address them. If that’s you, please let us know!
Big thanks to the incredible Yoav Fisher for providing a sanity check :)
Disclosure – we don’t have any position in any of the companies mentioned in this post. All the information given here is strictly an opinion and should not be redeemed as any investment recommendation whatsoever.






Great article. Very interesting take on the hybrid model. I definitely think that the rise in popularity will drive more innovation
I learned a great deal from reading your article . Thanks so much Nadav! JoAnn