Digital Health Business – Dr. Deneen Vojta, former EVP R&D at United Health Group
New episode in Digital Health Business by Arkin Digital Health.
(“Miniseries of interviews with industry leaders, coming from different parts of the US healthcare ecosystem, hopefully to provide Israeli entrepreneurs, investors and the Israeli healthcare community insights on the business side of digital health.”)
This time we had the pleasure of having Dr. Deneen Vojta, who spent the last 16 years at United Healthcare, the largest non-governmental health insurer in the US and S&P’s 8th largest company.
Dr. Vojta is a physician, turned entrepreneur, selling her company to United and then having a pivotal role in the organization’s effort to provide better, innovative care.
We talked about how United has become much more than just an insurer (today UNG is actually the largest employer of physicians in the US), why generating robust evidence is so important when interacting with payers and how being scrappy is important for nimble players but there is also a limit to how slim you can be to keep payers excited to work with you.
You can listen to the interviews and follow the series via -
Also, if you are not already subscribed to this blog, you can use this link to easily receive new posts!'
Nadav: You have such a vast working experience, in particular spending the last 16 years within the largest health plan, commercial payer in the United States. Perhaps you can think about an occasion or two that really influenced you in a significant way in your journey?
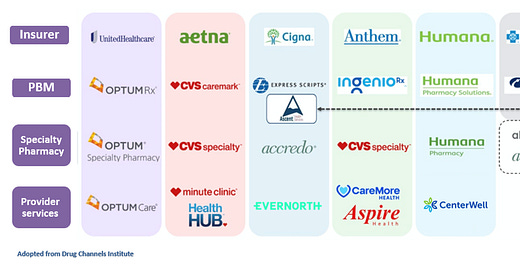
Dr. Vojta: Well, if you don't mind, I thought I would just start by telling your listeners a little bit about my history, because I think with that context you'll understand sort of the connection to UnitedHealth Group. And let me even make one small clarification as it relates to UnitedHealth Group. In reality, the Optum side of the House, which is both care delivery, consulting, service technology and of course the PBM is 50% of the House. And so it's not really just an “insurance company”. It is a large health and well-being company. And I think we're seeing a lot of that in the US marketplace that people are getting into each other's business in a way that's really exciting.
(The the next figure may add some color)
So let me back up a little. I trained at the Children's Hospital, Philadelphia in Pediatrics, and at the time the new CEO asked me to join his management team. So it was really kind of an exciting opportunity. And that was the beginning, frankly, of my administrative career.
And because I had an administrative day job, the best place for me to do my clinical practice was in the emergency room because it offered a lot of flexibility. And it was in the emergency room one night that I noticed that everybody in there, all these children had a lot of excess weight and I had never noticed all these overweight children. And in fact, all my years at job, I never had anybody ever talk about excess weight in children. I knew everything about complex cardiac disease or cancer or type one diabetes, but excess weight just was never discussed. And so I started doing a little homework on the Internet, and I noticed that the public health community had been ringing the bell about the increasing weight problem in the US for over a decade. But of course nobody was listening. And so I did some research and thought, well, if some parent did want help, where would I send them? And sure enough, there was a very strong evidence base, particularly for children under 12, that they do really well with weight loss. But there were really no services. So I decided that I would start a business in family weight management because it really is about the family. I tell you this story because when I think about your listeners, I think, you know, the context of a really good startup is, first of all, is there a need, is there a problem? And what was fascinating was that parents, particularly mothers, were very embarrassed about this. They knew the issue and really what they wanted. They wanted to make sure that that kid went to the prom, but they were embarrassed by it. So that was another learning about it. They didn't want to go into like the fat camp or to the fat doctor. Also, there was a strong evidence base. The American Academy of Pediatrics had really good guidelines showing and other research that proved that children who engage in healthy eating and activity actually can become normal weight in a couple of years. The key is before puberty because, as you know, through puberty we all become relatively insulin resistant. And that's why adults struggle with weight loss. And so anyway, I ended up starting a business and again learning from this sort of consumer insights that one, the mothers would pay for this too.
We decided to create a technology platform so that it could be done confidentially, anonymously, both telephonically and Internet based, which in many ways it was one of the first digital technology companies. And because of my academic roots, I was fixated on outcomes. So we were going to stick to the evidence and we're going to drive to the outcomes. And it turns out that that was a great idea because at the time UnitedHealth Group was getting into the wellness business and lo and behold, they needed a platform. So while we all think about selling businesses. I ended up selling capability… and again the need to understand what the problem is and will the market respond to it. And stick to the evidence.
Nadav: This is tremendous because all of these points are so relevant today. And I think so many companies can benefit from this mindset of crystallizing you’re the problem they are targeting and then generating the evidence either on the cost side or the clinical side of that problem, a very robust evidence that they are doing something significant. And then the question is, why is it significant and to whom? I mean, who should you approach with it? Maybe this can serve us as a segue way to speak about United a bit. And I guess on payers in general.
Everyone tries to understand how payers think. To your point Deneen, these are not just insurance businesses. I think today all of the large payers are essentially much more than just insurance. They're enabling and providing care in so many different ways. So when a company is trying to interact, let's say, with the health plan side of the business, what considerations entrepreneurs should have in mind?
Dr. Vojta - You know, it's a great question, and there's a lot of complexity in the US payer system. But the reality is and one can get lost in that kind of minutia, but the reality is that health plans all over the world want to pay for what works. And I think that's really critical. So that's why they're very focused, as we talked about, on the evidence base. Unfortunately, around the world and here in the U.S., we see a lot of low value health care, and it is often well published showing that something doesn't work. For example, we know that a lot of back surgeries are unnecessary and in fact you get much better outcomes from physiotherapy, yoga, etc. And yet, you know, for a long time the answer was to do a back surgery. If you could have asked a surgeon, well, does that back surgery, was it a success? And if the fusion took, yes, it's a success. But my back still hurts as the patient...
So that's why I think that the payers are very focused appropriately on how to eliminating low value care getting into the hands of patients, and enabling high value care as much as possible. And often that high value care cost more upfront. That's fine. But really it's about the (long term) evidence.
So if you're going to go to a payer you must actually have demonstrated outcomes in the published literature. So you can't just print a white paper and say, Hey, look at that and trust me, because we all need to have external validation for this kind of work. It's not just a nice to have. It's actually in the the payer certificate of coverage, which is filed with every state that experimental therapy is excluded. So they actually can't pay for it. And this isn't just the large commercial payers, this is also CMS because again, as a clinical priority and a fiduciary priority, we want to pay for what works. So focus on that…
Nadav: Let's spend some time on the Israeli angle. I know you had the opportunity to interact with a couple of Israeli companies. You've started to serve as an advisor and as a board member in a couple of companies. What are you seeing in Israeli companies?
Dr. Vojta: Let me start by saying in the last couple of years I read the books… for example The Start-Up Nation, which I'm sure many of your listeners have read, too. But I thought, first of all, it was well-written and a great articulation of both Israel itself and the Israeli people, you know, just truly impressive. And what I love about it is sort of they're the Israeli startups embracing of next gen(eration) technology, you know, so really thinking about the art of the possible, number one. Number two is I'm also impressed by, I daresay, but how much these startups are able to get done with more limited budgets than many organizations here in the US. I think that's really important and particularly in a startup community. And while it seemed less important for the last couple of years, I think the Israeli startups are in a good position because they've exercised that muscle of being prudent with their capital and that is really going to be incredibly important in the next couple of years.
Now, all that said, there's one small change I would recommend. I feel like and this is a number I'm just going to pull out, if they would spend 10% more, they could turn a minimal viable product into a minimal lovable product.
Nadav: I will try to be a bit Israeli and push you even further. I mean, for sure there are additional points that people can consider to be better. What else? I mean, frugal with capital, that's an advantage and sometimes disadvantage. What else?
Dr. Vojta: It's clear to me Israelis have a good understanding of their strengths. People are very proud of telling about where they spent their time in the military, whether they were in intelligence or they were in software engineering. You know, and really, it strikes me that because of their skill sets, they ended up being slotted into those positions. That's great. Know your strengths. But the flip side of knowing your strengths is being really aware of your blind spots. And so sometimes when I listen to the Israeli startup community speaking to the US customers, they're blind to how the American buyer thinks and just how the American buyer can receive information and what problems that buyer wants. Not what you may have developed as a solution (looking for a problem). You'll be far more successful if you think about the problem and then develop the solution.
Nadav: That’s great. Perhaps as a last questions let’s talk a bit on the market. We hear a lot about providers struggling, not recovering at the pace most people expected after COVID (if we can really say we are after COVID), i.e. not returning to the level of activity before COVID and especially not returning to same operational margins. But what about payers? I mean, I think 2020-21 were very good years for payers because of perhaps diminished level of care in some cases and lower payments as a by-product. How do you see payers in this current environment bouncing back from COVID?
Dr. Vojta: I'd say two big things jump out right away. One is, you know, we do have a problem around the world and particularly here in the United States with provider burnout. And when you listen to providers, one thing that comes out is the administrative hassles. And so on a very positive note, you see the payers and frankly the startup community beginning to focus on that. How to reduce the administrative burden and just the frustration and the harassment. So there is a real need for, I think, tech enabled service there. I mean, there still has to be an escalation pathway with human, but I think there's a tremendous opportunity to automate a lot more.
I'd say the second one is this whole notion of virtual care first. Well, almost overnight, a lot of visits went virtual. And to me it's particularly exciting when you can use the advances in telecommunications, all sort of technologies to allow me to interact with my doctor. And I think early days of telehealth were about getting some urgent care or less urgent. But what's I think really exciting is also the quick adoption of telehealth by everyday physicians from primary to specialty and behavioral health, of course, and to make that care more accessible. And now what again, I dare say, but particularly during the pandemic, that telehealth was used for access and now there's a laser focus on ensuring the same outcomes. Maybe in some cases we'll see better outcomes, but we don't know unless we study it. And of course from a service perspective, it feels like it is time to be much more consumer friendly.
Now, we can do this at much lower cost. So if my child has an ear ache and I think I need to go see an ENT physician, probably for the first visit a pediatrician will do a great job. And so that kind of steerage both saves of an unnecessary visit to a specialist and we can also then help make sure that that child can get seen in a timely way.
And payers get a bad rap here. Everyone wants to make it about the money. But the truth is, it is about the evidence and it's about the data…
If you are enjoying this blog, it would be really helpful if you can share it with relevant people.
Also, would love to hear your thoughts and feedback!
Thanks,
Nadav